OverviewAn aneurysm forms when there is a weakness between the layers of the artery. Shown is a normal artery and its three layers. An aneurysm can form either as a ballooning on one side of the artery or as a dilatation (enlargement) of the entire artery at a segment.What is subarachnoid hemorrhage (SAH)?Subarachnoid hemorrhage (SAH) is a type of stroke. Head trauma is the most common cause. Show
In patients without head trauma, SAH is most commonly caused by a brain aneurysm. A brain aneurysm is a ballooning of an artery in the brain that can rupture and bleed into the space between the brain and the skull. Risk factors for developing an aneurysm include:
Symptoms and CausesWhat are the symptoms of subarachnoid hemorrhage (SAH)?Most subarachnoid hemorrhages caused by brain aneurysms do not cause symptoms until they rupture. A ruptured brain aneurysm is an emergency and 9-1-1 should be called immediately. Symptoms of a ruptured brain aneurysm include:
Diagnosis and TestsCarotid and vertebral arteriesHow is a subarachnoid hemorrhage (SAH) diagnosed?
Other tests given after subarachnoid hemorrhage (SAH) is diagnosed The hospital care following the diagnosis of subarachnoid hemorrhage focuses on both discovering and treating the cause of the SAH, as well as managing its complications. Aneurysm detection Since brain aneurysms cause over 80 percent of nontraumatic subarachnoid hemorrhages, it is very important to image the brain’s arteries and then treat the aneurysm. The most common test performed to best see the brain’s blood vessels is a cerebral angiogram. A catheter is placed in the main artery in the groin (femoral artery) or wrist (radial artery). Through this a thinner catheter is advanced through the body’s arterial system into the neck. Contrast material is then injected and the X-ray pictures capture the blood flowing in the brain’s arteries and brains. Occasionally, subarachnoid hemorrhages may be caused by other brain or spine vascular lesions. An MRI of the brain and/or spine may be ordered if a cerebral angiogram does not demonstrate a brain aneurysm. A much rarer vascular cause for subarachnoid hemorrhage, benign perimesencephalic SAH is a type of SAH in which no vascular lesion is found on imaging. Some theories regarding cause include bleeding from a vein or from a blood clot in the blood vessel wall. Preventing aneurysm rebleeding Once an aneurysm has ruptured, there is an increased chance that it can rebleed. Brain aneurysm rebleeding is dangerous and can be fatal. The chance of rebleeding can be reduced by:
Management and TreatmentHow is SAH from brain aneurysm treated?Securing a brain aneurysm There are several ways to treat a brain aneurysm, including open surgery or endovascular treatment. Endovascular treatment of an aneurysm is a minimally invasive option using cerebral angiography to access the aneurysm. The decision on which treatment is best depends on the characteristics of the aneurysm and overall health of the patient. The surgical team will discuss these options and recommendations for which treatment is best. Open surgical techniques: clipping or bypass Clipping. One treatment for securing a brain aneurysm is through microsurgical clipping. This surgery requires a craniotomy. A craniotomy is performed by making an incision on the head and temporarily removing a small portion of skull. After the brain is exposed, the surgical team uses an intraoperative microscope to dissect through the brain to access the aneurysm. Once the aneurysm is visualized, a small clip is placed around the base, or neck, of the aneurysm. The skull portion is replaced and fastened with plates and screws, and the incision is closed.
Endovascular surgical techniques: coiling and/or stenting/flow diversion Endovascular treatment is a minimally invasive method to treat brain aneurysms.
How are possible complications from subarachnoid hemorrhage from brain aneurysm treated?Brain swelling and hydrocephalus Complications from SAH can include brain swelling and hydrocephalus. Bleeding from a subarachnoid hemorrhage can cause swelling of the brain, which can be life threatening. Monitoring of the brain’s pressure is important for any patient with symptoms of significant brain swelling. Medications can be used to treat brain swelling. Bleeding can also cause hydrocephalus, an excess of the cerebrospinal fluid (CSF) in the brain. Our brains float in a bath of CSF. This fluid is made primarily in spaces in the center areas of our brain called ventricles. The bleeding that occurs in SAH can cause an obstruction in the ventricles that blocks the fluid from passing through and these spaces get larger. This bleeding can also interfere with the brain’s ability to reabsorb the fluid normally. Hydrocephalus can be potentially dangerous if untreated. The treatment for hydrocephalus is to drain the excess fluid (see below). External ventricular drain (EVD). An external ventricular drain, or EVD, is a drain placed in the ventricle of the brain to serve both as a monitor for intracranial pressure (ICP), as well as a treatment for brain swelling and hydrocephalus. An EVD is placed by drilling a small hole in the skull and passing the catheter into one of the ventricles in the brain (shaded area of brain in illustration). Most patients have an EVD for 1 to 2 weeks. As the blood in the cerebrospinal fluid (CSF) clears, the team will attempt to “wean” the EVD by draining less fluid and determining if the patient can circulate and absorb their CSF normally. Shunt surgery. Most patients need an EVD temporarily until the brain can resume the regular flow and absorption of CSF. For some, the blood interferes with brain's normal absorption of CSF. If this occurs, a surgery called a shunt placement is recommended. A shunt surgery permanently places a drain from the ventricles into the peritoneal cavity of the abdomen to treat hydrocephalus. Seizures A seizure is an over-excitability of a brain cell’s electrical discharges. A patient can have a seizure that causes shaking of one part or all of the body. Or “silent” seizures may occur, which may cause sleepiness but are not otherwise clinically detected. After a subarachnoid hemorrhage, a patient may have a seizure from the sudden increase in brain pressure, or due to the bleeding in the brain irritating the brain cells. Patients are treated with medications to prevent them from seizing at the onset of the hemorrhage. They may also require longer-term therapy based upon the treatment and whether or not they actually seize. Some patients require monitoring for seizures with an electroencephalogram (EEG). An EEG is a test that uses electrodes temporarily attached to the scalp that show abnormalities in the brain’s electrical activity. Vasospasm and treatment methods After an aneurysm ruptures, the brain’s arteries may begin to narrow due to the presence of the blood and inflammation. This condition is called vasospasm. If the vasospasm is significant (called clinical vasospasm), a patient may develop neurologic changes and even suffer an ischemic stroke. The peak period for development of vasospasm occurs between the 7th and 10th days after the aneurysm bleeds, but may extend to 14 days or longer after the hemorrhage.
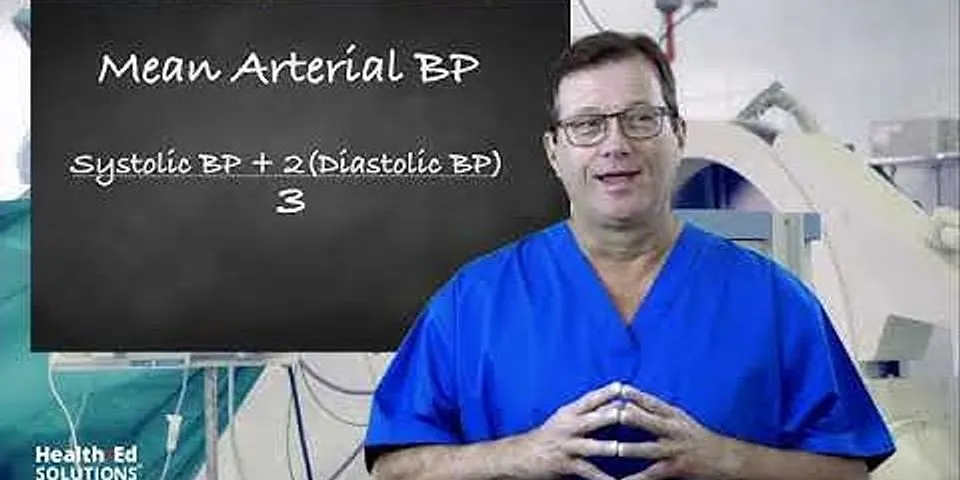
If a patient develops clinical vasospasm a number of medical measures are put in place to optimize oxygenated blood flow delivery to the brain in the intensive care unit. A cerebral angiogram may also be needed to treat vasospasm.
How long are hospital stays for subarachnoid hemorrhage (SAH)?Length of stay in the hospital varies based on patients’ clinical status. Most patients are admitted in the hospital anywhere from 10 to 20 days based on their condition, need for rehabilitation, and the presence and/or course of vasospasm. Patients diagnosed with benign perimesencephalic subarachnoid hemorrhage are usually discharged within 1 week. Living WithWhat follow up is needed after subarachnoid hemorrhage (SAH)?Patients are often seen in outpatient neurosurgical follow up after 1 month with a CT brain to evaluate neurologic recovery and evaluate for delayed hydrocephalus. Hydrocephalus can occasionally occur weeks after a hemorrhage if there is slow imbalance between the brain’s production and reabsorption of cerebrospinal fluid. Additional follow up with aneurysm imaging depends on the aneurysm’s initial treatment and the appearance of the aneurysm at discharge. It is important to maintain a long-term relationship with the cerebrovascular neurosurgical group for aneurysm monitoring. What is recovery after a subarachnoid hemorrhage (SAH)?Recovery after a subarachnoid hemorrhage widely varies based upon the cause and the extent of neurologic injury. Most patients with subarachnoid hemorrhage from an aneurysm require inpatient rehabilitation after the hospital stay, as well as outpatient therapy for months following. Feeling sad or anxious about the hospital stay or the illness is common. It is important to discuss these feelings with friends and family, as well as the medical team. ResourcesCleveland Clinic Stroke Support Group. The Cleveland Clinic offers a stroke support group which meets regularly. For more information about the support group, click link above or call 216-636-0450. Annual Cleveland Clinic Brain Aneurysm Awareness Run/Walk. The Cleveland Clinic hosts an annual brain aneurysm charity walk and run. This is also a great way for patients and families to celebrate survivorship and honor patients. All proceeds benefit patient resources and aneurysm research. For more information, click link above or call 216-623-9933. Outside brain aneurysm support information
How does brain injury affect blood pressure?Causes of High Blood Pressure After Head Injury
The medulla can no longer detect signals from the baroreceptors telling it to dilate the arteries. Damage to the rest of the brain makes the brain stem think the body is in distress, causing it to raise blood pressure.
How do you control blood pressure after brain injury?In general, the treatment of acute hypertension in patients with traumatic brain injury is not recommended. In terms of treatment, studies suggest that aggressive correction of out-of-hospital hypotension using normal saline solution, lactated Ringer's, hypertonic saline solution, or blood products improves outcome.
When do we consider lowering the blood pressure of a TBI patient?Importance Current prehospital traumatic brain injury guidelines use a systolic blood pressure threshold of less than 90 mm Hg for treating hypotension for individuals 10 years and older based on studies showing higher mortality when blood pressure drops below this level.
Can a brain injury cause high blood pressure?Severe traumatic brain injury (TBI), concussion (mild traumatic brain injury or mTBI), and other head trauma can cause high blood pressure, low blood pressure, and other circulatory system changes.
|